INTRODUCTION
Celiac disease (CD) is a genetic autoimmune condition linked to the HLA-DQ2 or HLA-DQ8 haplotype and affects millions of people worldwide. People of all ages suffer from it, although it is more common in women. Roughly 1 in 100 people in the United States have CD, but in countries like Saudi Arabia, Sweden, India, and Algeria, the seroprevalence ranges from 2.1%–8.5% (Singh et al., 2018). It is triggered by the consumption of gluten, a protein found in cereal grains such as wheat, barley, and rye. For this reason, people with CD must eliminate gluten completely from their diet and establish a gluten-free diet (GFD). A lifelong GFD is the only treatment. However, this presents many challenges. Gluten is found in nearly every type of food because of its versatile structure, leading to fear of gluten exposure when dining out or traveling. If a person with CD consumes gluten, it will lead to an immune-mediated response that attacks the villi in the small intestine, causing villous atrophy and preventing absorption of key nutrients. Over 200 symptoms can be linked to CD, ranging from classical symptoms (malabsorption, diarrhea) to nonclassical (anemia, neurological disorders) to asymptomatic (no symptoms) (Caio et al., 2019). The large variety of symptoms can make it difficult to diagnose, which often leads to misdiagnosis because many of these symptoms overlap with other medical disorders. As a result, most people go undiagnosed for 6-10 years, exacerbating their suffering and delaying appropriate treatment.
MISCONCEPTIONS/MYTHS ABOUT CD AND THE GFD
Misconceptions surrounding CD are largely due to a lack of awareness and education among both medical professionals and the general population. One of the most common myths is that CD can be outgrown. For years, medical professionals believed that CD was a childhood disease and would resolve over time, or go into ‘remission,’ because symptom severity would lessen with age. However, we now know that this is false – CD is a hereditary condition that can be activated by environmental triggers, but once active, cannot be reversed (3 Myths About Celiac Disease, 2022). Another common misconception surrounding CD is that it occurs mainly in those of European descent. This was a common belief throughout the 20th century, but countless recent studies have proven otherwise. This research has indicated that celiac, while common in Europe, is quite prevalent in Northern India and North African countries. However, a major obstacle in this epidemiological research is limited testing in Asian and African countries (Silvester et al., 2021).
Additionally, the idea that a gluten-free diet (GFD) is healthy for everyone is a false idea that has been spread mainly through the media. The GFD is currently the only treatment for CD, along with other gluten/wheat-related disorders such as gluten ataxia, non-celiac gluten sensitivity (NCGS), and others. At the same time, there are countless healthy individuals who also choose to eat gluten-free for their own personal choices. This trend is mainly seen among wealthier individuals, as gluten-free food tends to be more expensive. The GFD has been promoted as a weight-loss, or healthier diet, by influencers or celebrities. There is no evidence that shows that the GFD is beneficial for everyone. Gluten-free food generally has less nutrients (less iron, calcium, vitamins, etc) and contains more highly processed ingredients with added sugar, fat, and sodium. This can lead to obesity, cardiovascular complications, and other health issues (Makovicky et al., 2020).
Many people also believe that people with CD cannot touch gluten. A reaction can only be triggered in people with CD if gluten is ingested – gluten cannot be absorbed through the skin. However, some people with CD have dermatitis herpetiformis, a skin reaction of CD. People with this condition cannot touch gluten, but only roughly 1 in 10 people with CD have dermatitis herpetiformis (9 Questions About Celiac Disease, Answered, as Featured in USA Today | Celiac Disease Foundation, 2016). Finally, it is also a common idea that food labeled gluten-free contains no amount of gluten. While one may think that a food labeled “gluten-free” doesn’t contain gluten, the FDA requires that “gluten-free” foods contain 20ppm (parts per million) of gluten or less, leading to the FDA declaring 20ppm as the safe threshold for gluten-free foods. However, some tests are sensitive enough to detect as little as 3-5ppm and different gluten-free certification symbols can indicate varying amounts of gluten in ppm (The FDA’s Ruling on Gluten-Free Food Labeling | BeyondCeliac.Org, n.d.). Some people with CD may also react to smaller amounts of gluten, causing confusion among the CD community.
LITERATURE REVIEW
PATHOPHYSIOLOGY
CD is a complex disorder, therefore, it is important to understand the autoimmune reaction when a person with CD ingests gluten. A paper published by Posner and Haseeb in 2025 explains the pathophysiology, or autoimmune response, that occurs in individuals with CD. Gliadin, a key component of gluten, initiates this immune response. As a person with CD ingests gluten, the gliadin remains only partially digested when it reaches the small intestine because the peptides resist further digestion. The gliadin permeates the epithelial layer (the outermost of the small intestinal cells), and moves into the lamina propria – the next layer. In the lamina propria, tissue transglutaminase (tTG) will deamidate the gliadin. tTG is an enzyme that facilitates biochemical reactions. Deamidation is where a part of the amino acid is removed from the gliadin, mutating it.
The modified gliadin triggers an autoimmune cascade, producing various antibodies—some attack intestinal cells, while others cause inflammation. The tTG-IgA complex is also formed, which is one of the key components in diagnosing CD (Posner & Haseeb, 2025). This complex reaction results in villous atrophy – the destruction and flattening of the villi in the small intestine. The villi play an essential role in nutrient absorption. They are small, finger-like projections that line the small intestine and absorb key nutrients such as iron and vitamin B12. When the villi are flattened, their surface area decreases, limiting the crucial intake of vitamins. While gluten is the direct trigger, various factors contribute to disease onset.
CAUSES
CD is caused by the consumption of gluten and genetic and environmental factors. A paper by the AGA in 2020 (American Gastroenterological Association) explores the causes and diagnosis of CD. To have CD, one must have either the HLA-DQ2 or HLA-DQ8 genes. While over a third of people carry HLA-DQ2 or DQ8, only about 1% develop CD, suggesting that environmental triggers such as infections, microbiome, or gluten quantity/timing are also key contributors. A more significant amount of gluten consumed is associated with a higher risk of CD. Non-gluten-related factors might involve antibiotics, epigenetics, etc., although the exact mechanisms remain unclear. First-degree relatives, women, and individuals with other autoimmune diseases also face an increased risk (Lebwohl & Rubio-Tapia, 2020). While one must be eating gluten to have CD, there are still many factors involved, and it is uncertain how different environmental factors could play a role or trigger the disease. CD can also be developed at any age (even though it was previously considered a childhood disease), which suggests that additional influences contribute to the onset of this mysterious condition. Understanding the causes of CD is crucial, but recognizing its symptoms is equally important for early detection and management.
SYMPTOMS
There are over 200 possible symptoms of CD, categorized into classical, nonclassical, and silent CD. According to an article by the Celiac Disease Foundation, classical CD is classified by malabsorption, including diarrhea, weight loss, and stunted growth. These are traditional signs of CD. Nonclassical symptoms cover a variety of manifestations that are less clear or defined and may appear unrelated. They include anemia, abdominal pain, increased risk of bone fracture, anxiety/depression, skin rashes, and dental defects. Silent, or asymptomatic, CD occurs when there are no symptoms, yet villous atrophy is still occurring, and the patient could still face long-term effects of CD if undiagnosed (Celiac Disease Foundation, 2018). The sheer number of possible signs of CD exacerbates the challenges of obtaining an accurate diagnosis. Because of this, according to the Celiac Disease Foundation, the average time it takes to be diagnosed with CD is 6-10 years (9 Questions About Celiac Disease, Answered, as Featured in USA Today | Celiac Disease Foundation, 2016).
DIAGNOSIS
CD is typically diagnosed through a blood test (serology) and an endoscopy of the small intestine. A report published in 2024 by Elizabeth Wall and Carol E. Semrad in Current Gastroenterology Reports briefly explains the diagnosis of CD. Usually, a patient with suspected CD is tested through a blood test that detects the tTG-IgA antibody formed in those with CD. For this test to be accurate, one must eat gluten-containing products because this complex is only formed when someone with CD consumes gluten. If the blood test is positive, most patients follow up with an endoscopy of the small intestine to confirm villous atrophy.
Genetic testing is also used to aid in diagnosis, but mainly to rule out CD because one can’t have CD without the HLA-DQ2/8 gene (Wall & Semrad, 2024). Benjamin Lebwohl and Alberto Rubio-Tapia’s review explains the diagnosis of CD as well. They explain that the tTG-IgA blood test has a sensitivity and specificity of approximately 95%, meaning it correctly identifies about 95% of people with celiac disease and correctly excludes 95% of those without the condition. Intestinal biopsies also demonstrate approximately 95% accuracy and are typically used to confirm CD, while genetic testing can be used to evaluate individuals already on a GFD for possible CD (Lebwohl & Rubio-Tapia, 2020). The diagnosis of CD is relatively simple and highly accurate. However, early diagnosis is essential because the longer a person waits to be diagnosed, the more damage will be done, and the older a person is, the less likely they will recover.
The prevalence of CD also varies per country due to diet and amount of testing, and the prevalence has increased drastically over the past few decades. A review published by Simona Gatti in Gastroenterology AGA explores the epidemiology of CD in different countries. CD typically affects between 0.7% to 2.9% of the population and is more common in countries such as Finland, Italy, Canada, Asian countries such as India, and a group in Africa called the Saharawi. CD prevalence varies per country and mainly depends on gluten intake (Gatti et al., 2024). However, due to a lack of testing, the incidence of CD is unknown in many countries. Increased testing and consumption of gluten-containing products could be leading to an increase of CD around the world.
THE GLUTEN-FREE DIET (GFD) AND EFFECTS OF CD
Adhering to a strict GFD is among the greatest challenges of CD and a major contributor to reduced quality of life. Gluten is a protein found in grains such as wheat, barley, and rye. Because of its versatile behavior, gluten can be found in many different products, including salad dressing, ice cream, and shampoo. This can make it extremely difficult to avoid since gluten is involved in almost every aspect of our lives. Consequently, a strict GFD can lead to negative social, emotional, mental, physical, and even financial effects.
A research paper conducted by Sadaf Hameed and Vanita Sondhi in India explored the physical, emotional, and social effects of the GFD in children and adolescents by interviewing them. One participant explained, “‘When we go out, society sees us differently. We can’t tell everybody that I can’t eat wheat. I feel weird.’” Another participant shared the physical effects of this disease. “‘Earlier, when I used to do any work, I got tired, and my legs hurt a lot. Due to the pain in my legs, I used to come on the verge of crying.’” (Hameed & Sondhi, 2024).
Stroebele-Benschop’s study also explores the challenges of the GFD in those with CD and how it varies depending on the time of diagnosis. The results of this study show that the most challenging aspect is eating outside of the home. It also shares that the quality of life in those with CD is impacted by age, compliance, financial means, time since being diagnosed, the social-emotional implications of a strict GFD, and more. And, even though things improve with time (such as the ability to advocate for oneself), it is clear that many of these impacts continue to lower the quality of life of those with CD (Stroebele-Benschop et al., 2024).
Another study published by Bara Aljada shares some specific challenges of the GFD, such as the financial cost. “In one study, gluten-free products were 242% more expensive than their gluten-containing counterparts in the same food group” (Aljada et al., 2021). The high cost of a GFD adds to the financial strain for many families. Given these challenges, researchers are actively exploring alternative treatments that could reduce dependence on a strict GFD.
THERAPIES/FUTURE CURES
Scientists are researching various treatments that could improve the lives of those with CD. A review written by Franziska Buriánek explains some of the possible future therapies for this autoimmune disease. One of these ideas is the modification, or neutralization, of gluten. This would break down gliadin enough that it would lessen the effects of consuming gluten in those with CD. However, these drugs have shown mixed results, and it is unclear how effective they are. Another proposed idea is induced tolerance to gluten, which could allow those with CD to consume gluten (Buriánek et al., 2024).
A review by Amin Abbasi explores some more of these therapies. Other ideas include blocking the HLA-DQ2/8 genes, inhibiting the tTG enzyme, or genetically modifying gluten to make it easier to break down before reaching the small intestine. Abbasi also proposes the idea that probiotics or prebiotics could play a role in CD treatment/therapy (Abbasi et al., 2023). These potential therapies have much promise, but more research is required to develop a cure.
MATERIALS AND METHODS
This study used a quantitative survey to assess public knowledge and misconceptions about celiac disease (CD). The survey was distributed using Google Forms and automatically recorded participants’ email addresses and age range. No personally identifiable data were used in analysis, and participants were informed that their responses would remain confidential. The survey remained open for 64 days. It included 20 questions: 17 multiple choice, 1 select-all-that-apply, and 2 free response. A total of 162 respondents (n = 162), ages 13 and older, completed the survey. The majority of participants were students, as the survey was distributed at Madison West High School in the state of Wisconsin and through various media platforms. Of the participants, 51.9% were between the ages of 13 and 17, and 18.5% were between 18 and 24.
Three questions focused on demographics and perceived knowledge (e.g., age, self-rated knowledge of CD, and personal familiarity with someone who has CD). Other questions tested factual knowledge (e.g., prevalence of CD) and addressed common misconceptions (e.g., “Can CD be outgrown?”). Participants were required to complete all questions, and the average time to complete the survey was approximately five minutes. Responses were analyzed for patterns of misconception and trends in accuracy using the bar graphs created by Google Forms. Data were visualized using bar graphs to illustrate response distributions.
RESULTS
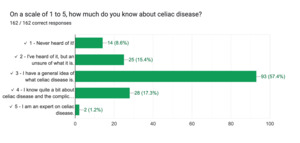
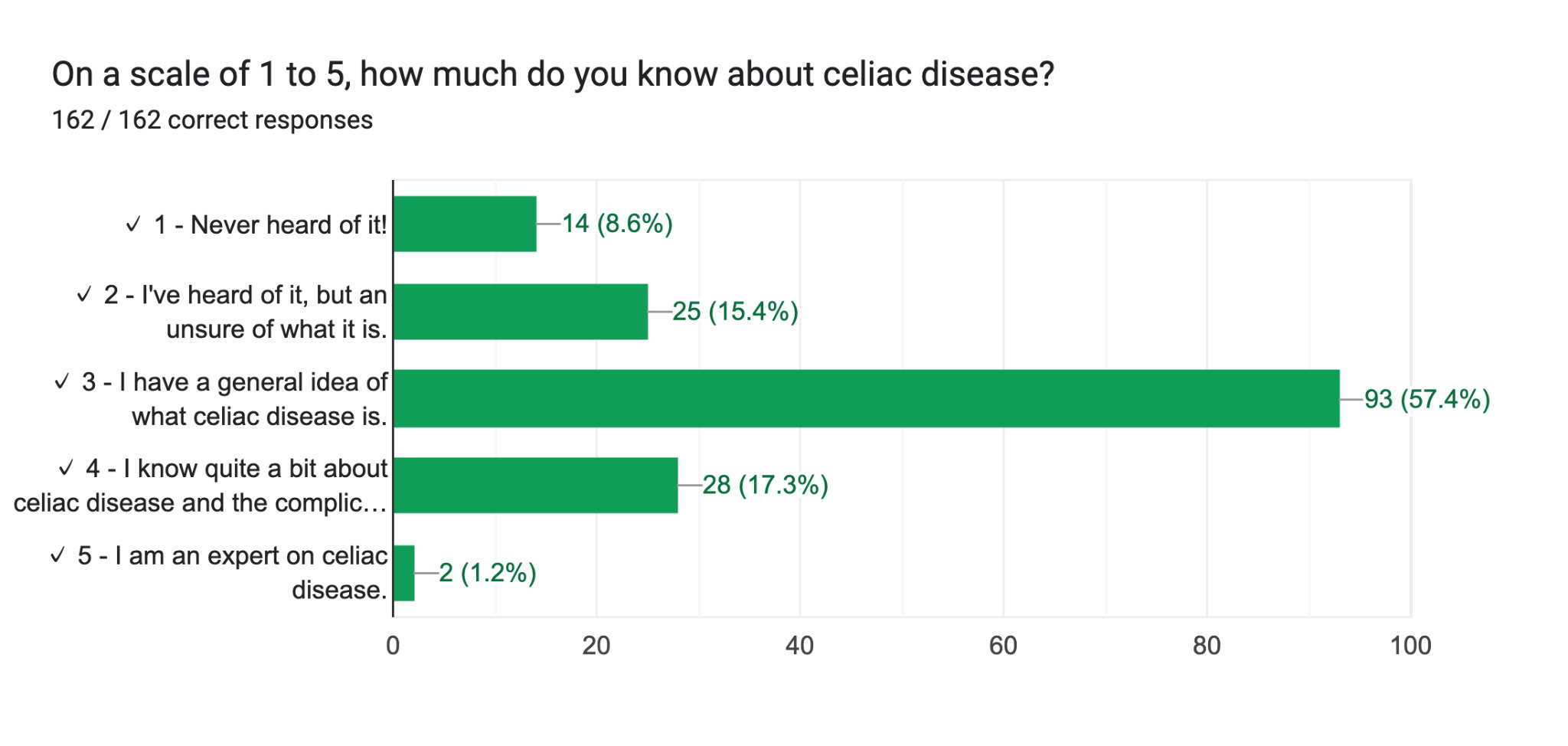
In this survey, there were 162 respondents that filled out a 20 question Google Form survey over the course of 64 days. Of these, 51.9% were aged 13–17, 18.5% were aged 18–24, 4.9% were aged 25–34, 6.8% were aged 35–44, 11.1% were aged 45–55, and 6.8% were aged 55 or older. Out of all respondents, 57.4% claimed to have a general understanding of celiac disease (CD), 24% were unsure or had never heard of it, and 18.5% reported above-average knowledge. Additionally, 65.4% of participants reported knowing someone with CD. In terms of dietary misconceptions, 21% of participants believe that a gluten-free diet (GFD) is healthy for everyone. Regarding disease classification, 19.1% of participants confused CD with an allergy. Over 75% correctly identified CD as an autoimmune disease, and small percentages confused CD with a virus (1.2%) or an infection (1.9%).
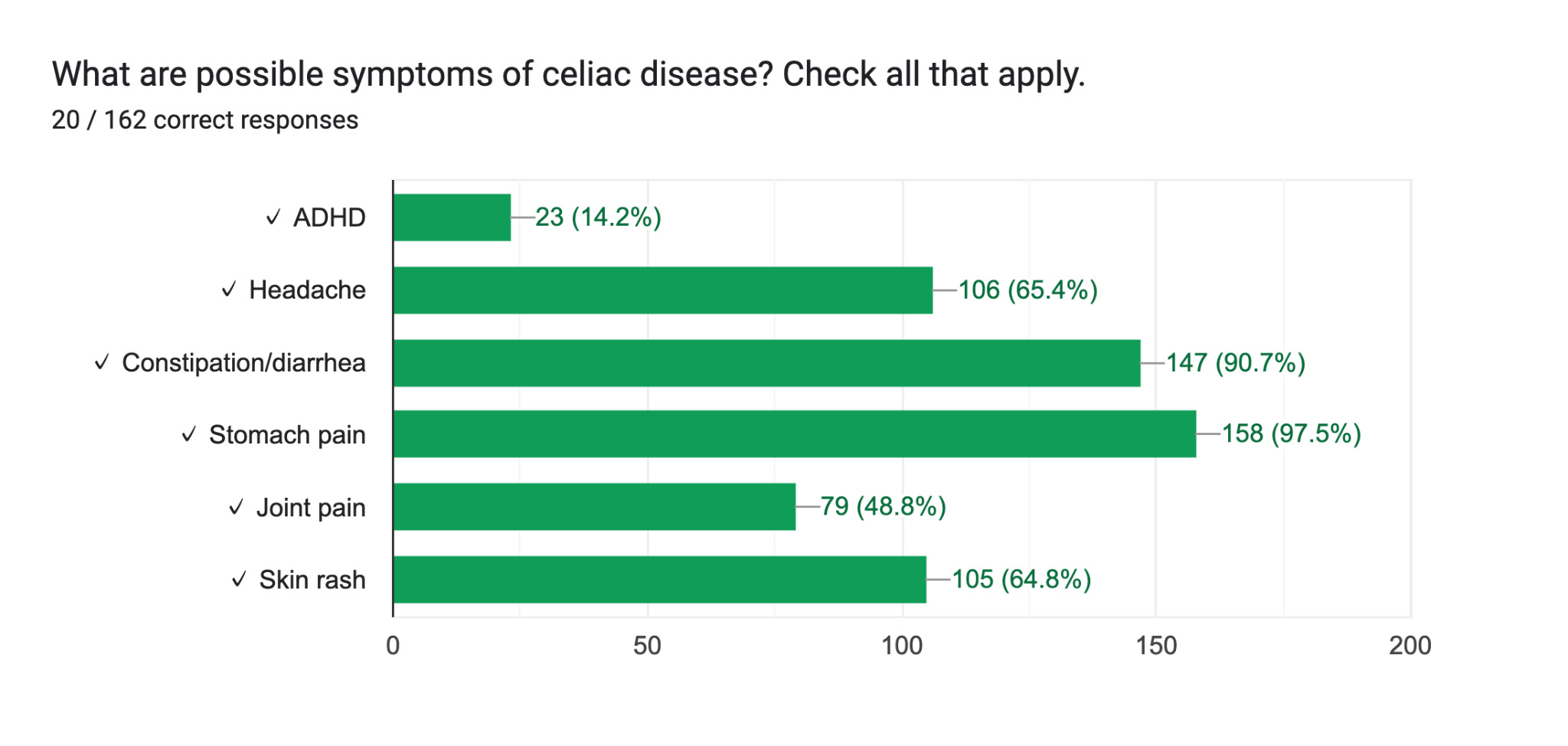
Knowledge of CD symptoms was also limited, as respondents frequently failed to identify the wide range of symptoms associated with the disease (Figure 2). Additionally, 26.5% incorrectly believed that CD damages the stomach rather than the small intestine (61.7% answered correctly). Misconceptions about the nature of CD were also evident in responses to questions about disease progression and diagnosis. For example, 22.8% believed that CD can be outgrown, and 79.1% did not know that it typically takes 6–10 years to receive an accurate diagnosis. Finally, 29.6% of participants incorrectly believed that people with CD cannot touch gluten.
These results reveal both areas of persistent misconceptions and perceptions of CD in the general public.
DISCUSSION
This research was conducted to address the lack of public awareness about celiac disease (CD) and the complications associated with it, particularly regarding its severity and prevalence. This study explored what the general population knows about CD and aimed to educate participants by providing explanations after survey completion. The results revealed that many people believe the common misconceptions associated with CD, despite the majority of participants claiming to have a fair understanding of the autoimmune disease. However, the survey helped to educate the participants after they filled it out by sharing the correct answer as well as an explanation for that answer. This helped to educate those who took the survey, leaving the participants more informed about CD and aware of the false ideas that surround the condition.
Four-fifths of the respondents claimed to have a general understanding or better of CD which means that the public is more informed than was expected. However, the results indicate that, despite the majority of the participants claiming this, most of the participants do not actually demonstrate at least a baseline awareness of CD. One of the respondents commented “I thought I knew a lot but just from taking the survey I see how little I know.” One-fifth of the participants also believed that a gluten-free diet (GFD) is healthy for everyone, a common but controversial idea. A GFD can help with other health conditions, but overall a GFD often contains more sugar, starch, and unhealthy fats. It has often been promoted as a weight-loss diet, when it more often leads to weight gain. Such misconceptions contribute to public misunderstanding, making it more difficult for individuals with CD to advocate for their needs. This result shows that the notion that a GFD is healthier is still prevalent. One participant commented “My best friend has celiac disease and so many people are misinformed about it because of fads and trends of the “gluten free” diet. It is such a struggle when we go out to eat at restaurants because even restaurants don’t always have the proper knowledge to be able to serve my friend.”
One of the most common misconceptions regarding CD, especially in the general public, is that CD is the same thing as an allergy. While 77.8% of participants correctly identified that CD is an autoimmune disease 19.1% confused CD with an allergy. This result shows that this is a common myth among the general public, leading to a misunderstanding of the disease itself. Another common mistake on the survey is that over a quarter of respondents incorrectly believed that CD damages the stomach. This may be because CD is associated with being a digestive condition, and when people think of digestion they typically think of the stomach. Although traditionally considered a digestive disorder, CD is increasingly recognized as a multisystem condition that affects various organ systems.
The results also signify that many misconceptions about CD remain prevalent to this day. Over 20% of the participants believed that CD can be outgrown, a myth that remains common even among medical professionals. CD cannot be outgrown as it is a genetic autoimmune condition. Nearly four-fifths of the participants were unaware that it typically takes 6–10 years to receive an accurate diagnosis of CD, highlighting the idea that the public is unaware of how little even medical professionals know about CD. Nearly a third of participants (29.6%) also incorrectly believed that people with CD cannot touch gluten. A person with CD can touch gluten, but cannot ingest it. This is important to be aware of because people with CD can be in an environment where gluten is prevalent (as long as it is not airborne).
The most significant result is surrounding the knowledge of CD symptoms. Many people were aware of the digestive symptoms of CD such as stomach pain (97.5%) and constipation/diarrhea (90.7%), while fewer participants recognized the more nonclassical symptoms that affect other body systems. This reinforces the common idea that CD is solely a digestive disorder. The second most commonly recognized signs were those that are often associated with other illnesses. This includes headaches (65.4%) and skin rash (64.8%). Nearly 50% identified joint pain as a possible symptom, but only 14.2% recognized ADHD as a possible symptom of CD. Some of the most common symptoms of CD are mental, including brain fog, ADD/ADHD, depression, and anxiety. These symptoms are often missed since they are not typically associated with CD.
The results of this survey align with previous studies, since they show that the public is often unaware of the misconceptions of CD and the symptoms associated with CD. Many people with CD are undiagnosed or misdiagnosed (around 70-80%), which could be due to the misconceptions surrounding CD symptoms and the idea that it is primarily a digestive disease.
CONCLUSIONS
These results expand on existing research that signifies the misconceptions and misunderstandings surrounding CD. They indicate that, while the general public believe they know what CD is, they are often misled by many common myths. Future experiments could focus solely on medical professionals to assess their understanding of the condition, or focus more on different types of misunderstandings surrounding celiac disease. To prevent this misinformation and encourage diagnosis in pediatric cases, doctors can recommend celiac screening for children who present with unexplained symptoms such as anemia, stunted growth, irritability, or chronic digestive issues—many of which are commonly overlooked. Since CD symptoms can appear vague or mimic other conditions, adding celiac testing to routine blood panels for children could help ensure earlier detection. New parents, in particular, may not be aware of the wide range of symptoms or the hereditary nature of CD. There are also many misconceptions regarding what races and ethnicities CD affects, which can lead to people of certain ethnic and racial backgrounds not getting tested. CD has a worldwide prevalence, so it is important that patients are tested for CD regardless of their background. Pediatricians can play a crucial role in bridging this gap by providing educational materials during early wellness visits and directing families to trusted organizations like the Celiac Disease Foundation. These proactive measures can empower parents to recognize symptoms early, ask the right questions, and advocate for proper testing and care.
Several national organizations are actively engaged in efforts to raise public awareness about CD. Among them, Beyond Celiac and the Celiac Disease Foundation (CDF) play prominent roles in promoting education, advocacy, and policy reform. Both organizations support initiatives aimed at improving gluten labeling regulations and provide opportunities for individuals to become CD advocates through structured outreach programs. The CDF, for example, offers “Team Gluten-Free,” a fundraising initiative that enables participants to support CD research and awareness efforts. Additionally, the foundation’s policy advocacy program equips individuals with training to promote community-level change through public education and legislative engagement. The CDF also encourages individuals with CD to participate in clinical trials to advance scientific understanding and foster broader awareness of the disease.
Beyond awareness campaigns from organizations like Beyond Celiac and the CDF, more systemic initiatives could help close the knowledge gap. For instance, public health campaigns during Celiac Awareness Month, school health curricula updates, mandatory CD training for medical professionals, and federal policies strengthening gluten labeling could improve early diagnosis and reduce stigma. Technology could also play a role – apps that verify gluten-free safety or AI-powered symptom trackers may empower patients and raise awareness. Currently, apps such as “Gluten-Free Watchdog” help people with CD manage a gluten-free diet (GFD) by providing information about what foods are gluten-free and food recalls. Additionally, “Find Me Gluten-Free” helps the user find restaurants that are safe to eat at based on customer reviews.
ACKNOWLEDGEMENTS
Thank you to my friends, family, and teachers who helped to distribute this survey and take it to test their knowledge of CD.
CONFLICTS OF INTEREST/DISCLOSURE
None.